It's weeks fourteen to sixteen but I've abandoned all that now...
I was pretty surprised to find I'd not written a blog with this title before given how obvious a statement it is. Better late than never I guess...
I actually started writing this a week ago and ended up with no time and no mental energy to give to it and so it sat as an ignored tab on my browser until now. Whilst it hasn't nagged at me, I've been glancing up from work and seeing it, not unfinished as much as not at all started and I think it's pushed me towards something to say.
I think a large part of my neuroses/anxiety/idiocy (delete as you see appropriate) comes from this inability to stop a half-thought from getting in my head and then being unable to stop myself following it through to some horrifically sad or depressing ending.
Whilst I don't like it, I'm prepared to make peace with the idea that this will happen if I'm consciously dwelling on something that I know is going to get me down. But where I really struggle is when it ends up in my head totally uninvited and I go from minding my own business to the depths of despair in the blink of an eye.
 |
| Going from 0-100 really quick |
I don't think these are 'intrusive thoughts', though there's maybe some overlap with that definition. And I'm loathe to start Dr Googling myself into oblivion and giving myself more labels than I need - I've got enough going on as it is.
But there is something there that I genuinely find difficult about my mind getting ahead of me and not being in total control of it. It feels decidedly unfair that a line in a song, a reference to a place on TV or even just a random word I overhear sends me spiraling and I just cannot control it.
Obviously I've learned how to manage it when I end up at Despair's Door and I have successful and unsuccessful days with that, but it seems like there should be more to head that off and stop it for getting to that point. I haven't found it yet.
So I started thinking about why all this happens - there must be something that subconsciously pushes those thoughts around. And as most things in life that hold us back are either fear or admin, and this isn't admin.. well that leaves fear.
So what am I scared of? Apart from confined spaces, spiders and large dogs?
 |
Help me
|
Definitely being alone. If this blog has highlighted anything over the last million weeks, it's that being left alone with my thoughts for any period of time is Not A Good Thing. I think there's also something about wanting to be, or to feel noticed, and that was a surprisingly difficult revelation this week.
We all have people we love and care about and those relationships shift over time. I think my realisation was that there's a fear that I won't be noticed the way I notice others. Or I won't be wanted, or cared about the way I do with others.
 |
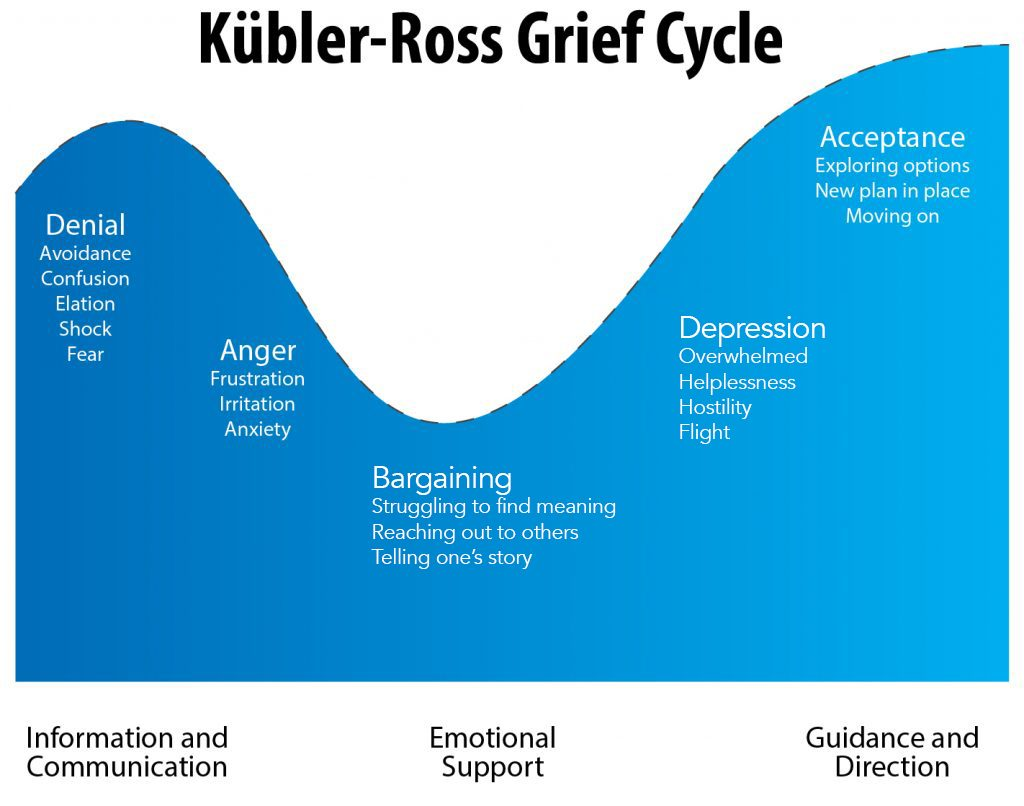
| Guess which one is the default? |
And so of course, a lot of people go straight for the rainbow, while I'm already halfway down the right-hand fork in the river, futilely paddling against the current. At CBT we talked a lot about how valuable inter-personal relationships are and how the 'intimacy' (and by that I mean closeness, vulnerability, honesty etc here) is important for us.
I guess the fear then comes from knowing that and then thinking that what you have or perceive isn't reciprocated or valued in the same way. Or that you'll do so much to validate it that you'll ultimately doom it to failure.
It's almost certainly unfounded. But that's really hard to reconcile. Really really hard. To the point where a crippling amount of time can end up being given over to the idea that I've irretrievably ruined a friendship or mortally pissed someone off who's realised that I'm not worth their time at all.
 |
So it stupidly feels like this
|
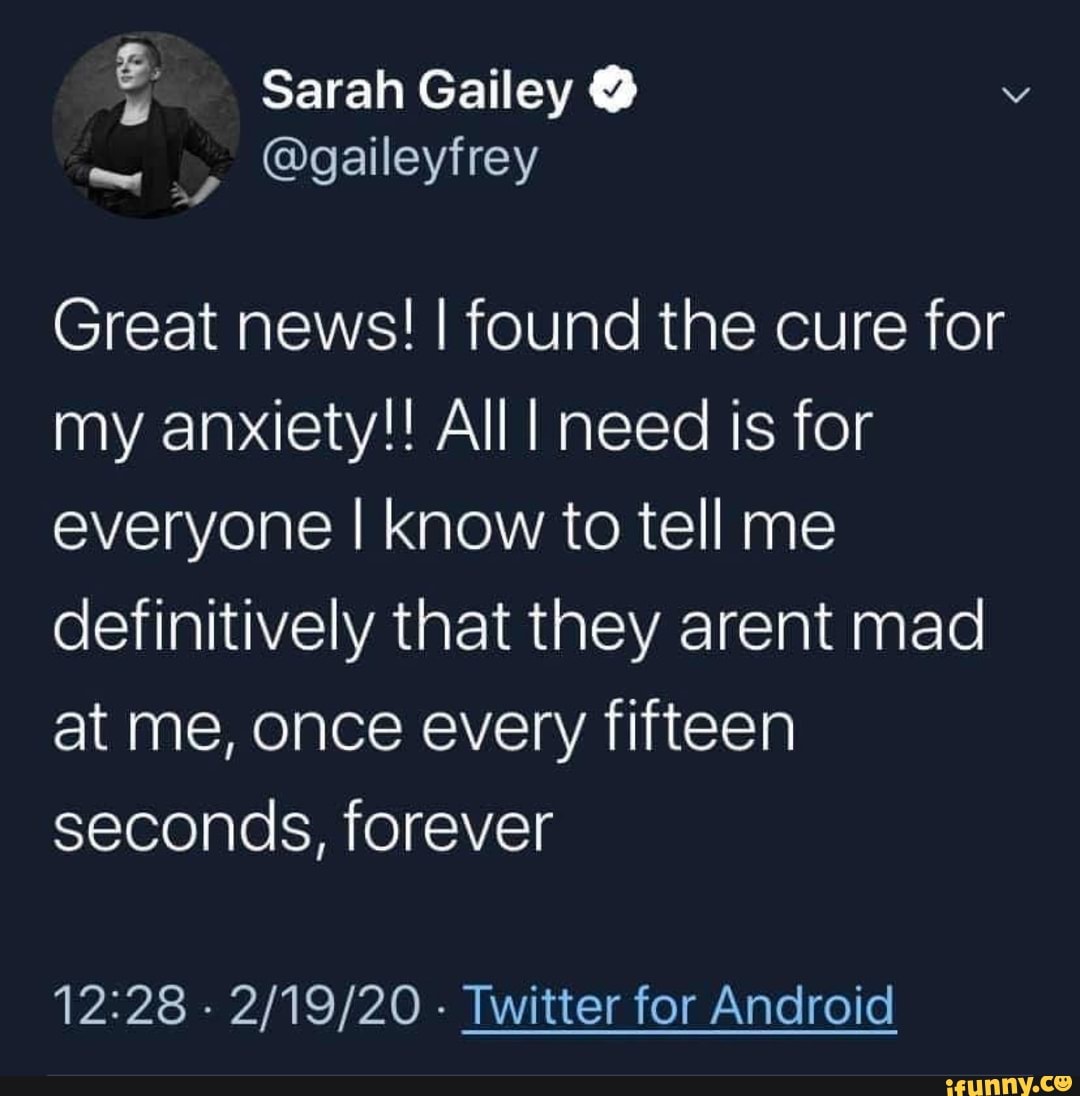 |
And here's one unhelpful solution
|
And of course nobody likes to feel like this, least of all me. And that's why it all feels so stupidly unjust that I can't prevent it from happening. It's easy to withdraw a lot and keep from taking the risk in the first place, but that's no real way to live your life is it?
I guess lockdown has helped me gradually figure some of this out over the last few months. But really being able to banish it feels a long way off.
I hope everything's OK between us. Sorry if not....
Until next time. Stay safe x